Category: Sci-News
-

Midnight’s Secret: The Hormone That Silences Your...
Continue ReadingMidnight’s Secret: The Hormone That Silences Your Hunger
What if the secret to preventing obesity lies not just in what we eat but also in how we sleep?
According to groundbreaking research, scientists have uncovered a new hormone called Raptin that spikes during our sleep and plays a critical role in controlling appetite and weight gain.
This finding could open doors to innovative therapies for those struggling with obesity, offering fresh hope rooted in our natural circadian rhythms.

Recent research identifies Raptin as a previously unknown hormone produced in the hypothalamus, the master control center of the brain that governs crucial functions like body temperature, hunger, and sleep.
It turns out Raptin is released primarily during the sleep phase—when its levels peak in the bloodstream—and its presence correlates with a notable reduction in appetite.
- In mouse models with disrupted sleep schedules (e.g., “sleep fragmentation”), scientists observed a decline in Raptin levels. This reduction corresponded with increased food intake, faster weight gain, and a higher propensity for obesity.
- Conversely, animals given extra Raptin or genetically engineered to produce more of it exhibited lower appetite, reduced body weight, and healthier metabolic markers.
These findings point to a strong link between sleep quality and metabolic health, offering a more complete picture of why poor sleep habits can accelerate weight gain.
Stay updated with top science articles and brief summaries delivered to your email!
Breakdown of Mechanisms:
1. Origin and Timing
a. Raptin is cleaved from a protein called RCN2 in a specific region of the hypothalamus known as the paraventricular nucleus (PVN).
b. Production is triggered by signals from vasopressin-producing neurons in the suprachiasmatic nucleus (SCN)—the “circadian clock” of the brain.
c. Because these signals are strongest during rest periods, Raptin levels naturally surge at night (or whenever an organism’s major sleep window occurs).
2. Binding and Action
a. Raptin attaches to a receptor named GRM3 in the hypothalamus and in certain neurons in the stomach.
b. Through this receptor, Raptin activates a biochemical pathway (involving PI3K-AKT signaling) that makes neurons more energetically “ready,” ultimately dampening the urge to eat.
c. Another effect is delayed gastric emptying, meaning your stomach sends “I’m full” signals for longer, naturally decreasing the desire for extra meals or snacks.
3. Real-World Consequences
a. If sleep is consistently cut short or is of poor quality, your body may not produce enough Raptin at night.
b. You might then wake up hungrier or feel compelled to snack more often—especially late in the evening—hastening weight gain.
c. Conversely, prioritizing adequate, high-quality sleep appears to boost Raptin levels and supports healthier eating patterns.
Impact on the Body and Daily Life:
a. Metabolic Benefits:
People (and animals) with robust Raptin rhythms tend to regulate blood sugar and insulin sensitivity more efficiently, indicating possible protection against type 2 diabetes.
2. Weight Management:
Raptin’s ability to curb appetite and slow gastric emptying points to potential new weight-loss or weight-maintenance strategies.
3. Mood and Wellbeing:
Better sleep is often associated with improved mood. While still under investigation, the synergy between balanced Raptin release, stress management, and emotional regulation may help curb some of the emotional-eating triggers.
Join our email list to receive job alerts directly in your inbox!
While more research is needed, the discovery of Raptin offers a unique view of the sleep–appetite connection. It suggests that getting enough rest isn’t just about recharging our minds—it might be vital for keeping our bodies at a healthy weight.
By taking steps to optimize sleep quality (think comfortable dark rooms and consistent bedtimes), you might help your body naturally sustain Raptin levels.
The next time you’re tempted to skimp on rest, remember: in addition to mental clarity, a good night’s sleep just might be your best ally in managing your waistline and overall health.
Share
Related Articles
Career Opportunities
Explore Science Stories
Recent Career Opportunities
-

How Exercise Can Delay Aging: Insights From...
Continue ReadingHow Exercise Can Delay Aging: Insights From a New Research

Imagine a world where aging doesn’t mean losing your ability to move freely or stay independent. What if the secret lies not in a bottle, but in the type of exercise you choose?
A groundbreaking study on mice reveals how exercise impacts aging—and the results may inspire a new fitness routine.
Stay updated with top science articles and brief summaries delivered to your email!
Key Findings:
1. Exercise Types Tested: Two exercise models were compared—High-Intensity Interval Training (HIIT) and Voluntary Wheel Running (VWR). HIIT involves intense bursts of activity followed by rest, while VWR mimics casual jogging where mice exercise at their own pace.
2. Impact on Aging: Both forms of exercise improved or preserved physical function in older mice, with significant reductions in age-related declines.
3. Key Results for Older Mice:
- Improved strength, endurance, and body composition.
- Maintained muscle function compared to sedentary counterparts.
The researchers used C57BL/6 mice—commonly used in aging research. Mice were split into three groups: HIIT, VWR, and sedentary controls.
Over 13 weeks, the team assessed physical performance using a comprehensive scoring system called CFAB, measuring strength, endurance, and overall mobility.
Breaking Down the Mechanisms:
HIIT’s Efficiency: Short but intense workouts led to substantial improvements in treadmill endurance and fat reduction in older mice.
Think of HIIT as sprinting up a hill and then walking down—it’s intense but quick.
VWR’s Consistency: This model showed more gradual benefits, such as better grip strength.
Picture a leisurely jog in the park—it’s less intense but still beneficial over time.
How Does This Translate to Humans?
1. Muscle Preservation: Aging humans lose about 1%–2% of muscle mass annually after 50. Exercise—regardless of intensity—can significantly slow this decline.
2. Time-Saving: HIIT offers similar benefits as traditional endurance exercise but requires less time—perfect for busy schedules.
3. Real-World Impact: Encouraging any form of physical activity can counteract age-related frailty, supporting independence.
Join our email list to receive job alerts directly in your inbox!
Practical Applications:
1. For Beginners: Start small. Even short walks or light jogging can bring noticeable benefits.
2. For Time-Conscious Individuals: Incorporate HIIT into your routine with just 20-minute sessions a few times weekly.
3. Diet Matters: Pair exercise with protein-rich diets to maximize muscle retention.
Relating to You:
Whether you’re a student, a tech worker, or a retiree, this study underscores one thing—starting any exercise routine, at any age, can be transformative. For older adults, even light activity can preserve mobility and improve quality of life.
Conclusion:
This study reaffirms an age-old mantra: “Move it or lose it.” But it also highlights that the how matters less than the doing. Whether you’re sprinting through HIIT or strolling in a park, every step counts toward aging gracefully.
Share
Related Articles
Career Opportunities
Explore Science Stories
Recent Career Opportunities
-

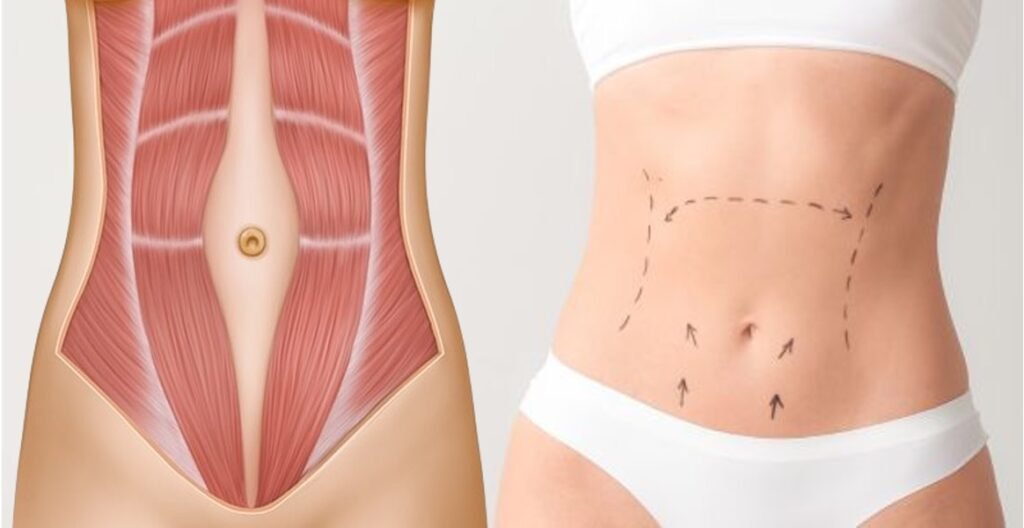
A Revolutionary Approach to Obesity Treatment
Continue ReadingA Revolutionary Approach to Obesity Treatment

What if managing your weight could be as simple as targeting two hormones? Imagine a future where obesity treatments are not just effective but sustainable and personalized.
A groundbreaking study published in Science Translational Medicine unveils a dual-action hormone therapy that could change the landscape of weight loss forever.
Stay updated with top science articles and brief summaries delivered to your email!
Obesity is one of the most challenging health crises of our time, with millions struggling against its effects. Traditional approaches, from diets to medications, often fall short of long-term success.
Scientists have long known about two key players in regulating our metabolism: glucagon-like peptide-1 (GLP-1) and leptin. While GLP-1 helps control appetite, leptin signals the brain about the body’s fat stores.
But here’s the catch: these hormones have limitations when used individually. That’s where this research takes a bold step forward: combining the powers of GLP-1 and leptin into a single therapy.
What’s more, the study identifies specific neurons in the brain that make this therapy work—a discovery with profound implications for treating obesity.
Researchers designed a dual agonist molecule targeting receptors for both GLP-1 and leptin. Here’s what they found:
1. Enhanced Weight Loss: The dual therapy was significantly more effective at reducing food intake and body weight compared to using either hormone alone. Mice treated with the dual agonist showed sustained weight loss over several weeks.
2. Precise Targeting: The therapy works by acting on neurons in the hypothalamus—a brain region critical for appetite and weight regulation.
3. Broad Applicability: The findings were consistent across different mouse models, including those resistant to leptin alone.
Think of GLP-1 and leptin as two keys that unlock different doors to weight control. GLP-1 focuses on immediate hunger signals, while leptin manages long-term energy balance. By combining these keys into one therapy, the dual agonist effectively “hacks” the brain’s appetite control system.
To understand this better, imagine the hypothalamus as a thermostat for your body’s energy. The dual agonist resets this thermostat, helping the body maintain a healthier balance between energy intake and expenditure.
The practical applications of this therapy are far-reaching:
1. Personalized Medicine: Since the dual agonist targets specific neurons, treatments could be tailored to individual metabolic profiles.
2. Long-Term Success: Unlike current therapies that lose effectiveness, this approach has the potential for sustained weight loss.
3. Lifestyle Integration: Future treatments may involve a combination of this therapy with dietary and behavioral interventions.
Join our email list to receive job alerts directly in your inbox!
The dual agonist could revolutionize how we approach obesity:
1. Medical Therapies: New weight-loss drugs may emerge, offering more effective and less invasive options.
2. Proactive Health Management: By reducing the risk of obesity-related conditions like diabetes and heart disease, this therapy could significantly lower healthcare costs.
3. Accessible Options: The research opens the door for treatments that cater to those with obesity-resistant metabolisms.
This research not only provides hope for millions struggling with obesity but also sets the stage for a new era in metabolic health. By targeting both immediate and long-term regulators of energy balance, the dual agonist represents a leap forward in therapeutic innovation.
What could this mean for you? As scientists refine this approach, we may soon witness treatments that are both highly effective and widely accessible. Are we on the brink of ending the obesity epidemic? Only time will tell—but the future looks promising.
Share
Related Articles
Career Opportunities
Explore Science Stories
Recent Career Opportunities
-

How Gut Microbiota and Circadian Rhythms Could...
Continue ReadingShare this news

What if the secret to managing stress wasn’t just about mental techniques or medications but about your gut?
Recent research reveals that the bacteria living in our digestive system could control how we handle stress throughout the day.
This breakthrough study from Cell Metabolism uncovers the powerful connection between gut microbes, circadian rhythms, and our body’s response to stress.
The study highlights a groundbreaking discovery: gut microbiota regulate stress-response hormones like corticosterone by syncing with the body’s circadian rhythms.
Researchers found that when gut microbiota were disrupted, such as through antibiotic treatment, the natural stress response became erratic.
This showed that the bacteria in our gut help maintain proper stress levels by aligning with our biological clock.
The gut microbiota display diurnal rhythms, meaning they fluctuate in a predictable pattern throughout the day. These rhythms help control the release of corticosterone, a hormone involved in stress responses.
When these microbial rhythms are disrupted, such as in germ-free or antibiotic-treated animals, stress hormones are released irregularly. This leads to heightened stress responses, particularly at times when the body typically expects a surge of stress hormones.
The research found that when the natural rhythms of gut microbes are disturbed, the body’s stress system—especially the hypothalamic-pituitary-adrenal (HPA) axis—fails to operate effectively. This could have real-world consequences, such as impaired stress responses, which may contribute to mental health issues like anxiety and depression.
This discovery opens up the possibility of developing probiotic-based therapies to improve stress management. By restoring the proper balance of gut bacteria, we might be able to support healthy stress responses and improve mental well-being. Probiotic treatments or even dietary changes that promote healthy gut microbiota could one day become a part of standard stress management strategies.
Imagine being able to manage stress simply by improving your gut health. This research suggests that what happens inside your gut is more powerful than you might think. By taking care of your gut, you may be able to support a healthier, more resilient stress response.
The study used animal models to show how the depletion of gut microbiota disrupted the natural rhythm of corticosterone release. For example, Lactobacillus reuteri, a strain of bacteria found in the gut, was shown to play a significant role in regulating these rhythms.
Understanding the connection between gut microbes, circadian rhythms, and stress opens a new frontier for managing mental health. Probiotic-based solutions could revolutionize how we handle stress in our fast-paced world.
As research continues, the implications for treating stress-related disorders are immense. What could this mean for you—could improving your gut health help you stress less?
Share this news
Related Science Stories
Recent Career Opportunities
-

Is Pollution Secretly Making You Diabetic?
Continue ReadingShare this news
Recent research unveils a startling link between air pollution and your body’s ability to regulate blood sugar and energy, potentially paving the way for metabolic diseases like diabetes.
The culprit? A common air pollutant known as benzene.
Benzene, a volatile organic compound (VOC), is a sneaky yet prevalent part of urban air. It’s released by vehicle exhaust, industrial emissions, and even everyday products like paint and cleaning supplies.
While its toxic effects on cancer risk are well-documented, scientists at Wayne State University dug deeper to uncover another alarming consequence: benzene may directly interfere with how our bodies maintain energy balance, starting with the brain.
The research focuses on the hypothalamus, a small yet mighty part of the brain responsible for controlling hunger, energy, and blood sugar. Using male mice as models, the scientists found that benzene exposure disrupted energy regulation through an unexpected player—microglia.
These tiny immune cells in the brain, typically the first responders to injury or infection, became hyperactive when exposed to benzene. This overactivation set off a cascade of inflammation in the hypothalamus, impairing insulin signaling and ultimately throwing the body’s metabolic balance out of sync.
Within days, the exposed mice showed spikes in blood sugar and significant disruptions in energy management, even without changes in their diet or physical activity.
Interestingly, the effects of benzene exposure were not universal. Female mice seemed to resist the metabolic disruptions caused by benzene. Scientists suggest that this resilience may be linked to hormonal differences, particularly the protective effects of estrogen, and differences in how male and female bodies metabolize benzene.
The researchers didn’t stop at identifying the problem—they also worked on solutions. By targeting a specific inflammation pathway in the microglia, called NF-κB signaling, they managed to prevent the harmful effects of benzene exposure.
This breakthrough suggests that therapies targeting this pathway could protect against metabolic diseases triggered by environmental pollutants.
This study is a wake-up call about the hidden health costs of air pollution. Benzene exposure isn’t limited to industrial settings—it’s part of our daily lives, especially in urban areas.
The findings underline the need for stricter air quality regulations and personal steps to minimize exposure. Using air purifiers, avoiding VOC-heavy products, and advocating for cleaner transportation policies are practical ways to protect yourself.
The air you breathe has a more profound impact on your health than you might think. This groundbreaking study not only uncovers how air pollution can sabotage your metabolism but also offers hope for preventive measures.
As we continue to explore the intricate connections between our environment and health, one thing is clear: cleaner air is essential for a healthier future.
Share this news
Related Science Stories
Recent Career Opportunities
-

What Happens Inside Your Muscles When You...
Continue ReadingShare this news
Prof. Samuel Klein and his team at Washington University in St. Louis embarked on a fascinating journey to uncover the hidden changes happening inside skeletal muscles of people with obesity and type 2 diabetes (T2D) after significant weight loss. Their findings could offer hope to millions battling the intertwined challenges of obesity and diabetes.
Type 2 diabetes often begins with insulin resistance in muscles — a condition where muscle cells fail to respond effectively to insulin, leading to high blood sugar levels.
Previous studies hinted that certain fat molecules, called ceramides, might play a critical role in this process. But which ones? And where in the muscle are they causing trouble?
To answer this, the researchers studied 14 individuals with obesity and T2D who achieved substantial weight loss (about 19% of their body weight) through diet or surgery.
Using advanced techniques, they examined the muscle cells for two key culprits: diacylglycerols (DAGs) and ceramides.
The team expected to see a dramatic decrease in all problematic lipids after weight loss, but the results told a more nuanced story.
While the levels of some ceramides in the muscle’s outer membranes remained unchanged, a specific type—C18:0 ceramide—hidden deep within the mitochondria (the cell’s powerhouse) and endoplasmic reticulum dropped by 20%. This reduction coincided with a remarkable doubling of muscle insulin sensitivity.
Prof. Klein explains, “Our study shows that reducing mitochondrial C18:0 ceramide may be a key mechanism through which weight loss improves muscle insulin sensitivity.”
Interestingly, another type of ceramide, C24:1, increased in various parts of the muscle. While its role isn’t fully understood, it seems to be less harmful than C18:0 ceramide, suggesting that not all lipids are villains in this metabolic drama.
This discovery highlights the intricate balance of bioactive lipids in muscle health. It suggests that targeting mitochondrial ceramides could offer new ways to enhance insulin sensitivity, potentially leading to better treatments for type 2 diabetes.
For now, Prof. Klein and his team emphasize the power of weight loss. “The metabolic benefits of significant weight loss extend beyond what we see on the scale, profoundly impacting cellular health and insulin action.”
This research serves as a reminder of how weight loss can transform the body from the inside out. It’s not just about numbers on a scale—it’s about empowering your cells to function better and protect you from chronic diseases.
So, the next time you lace up your sneakers or prepare a healthy meal, remember: your muscles are thanking you in ways you can’t even see.
Share this news
Related Science Stories
Recent Career Opportunities
-

Long-Lasting Weight Loss in a Single Shot?...
Continue ReadingShare this news
Imagine if a single injection could help people shed unwanted weight, control hunger, and improve their metabolic health—all with effects that last for months.
For millions struggling with obesity, this might sound too good to be true. But scientists may be on the verge of turning this vision into reality with a new, innovative treatment called AMG 133.
AMG 133 is not just any weight loss drug. It’s a combination treatment designed to tackle obesity at its root, working with the body’s natural systems for regulating weight.
Obesity has become a global health crisis, affecting hundreds of millions worldwide and increasing the risk of serious conditions like heart disease, diabetes, and stroke.
Standard treatments for obesity have helped some people, but they often require frequent doses or produce only limited results. AMG 133 aims to change that by offering a more effective and longer-lasting solution.
How Does AMG 133 Work?
AMG 133 is based on the combination of two natural hormones—GLP-1 and GIP. Each of these hormones plays a distinct role in managing appetite and energy storage. GLP-1, a hormone released after eating, signals fullness and encourages the body to burn energy rather than store it.
Because of these effects, GLP-1 treatments are already used for managing type 2 diabetes and, more recently, as weight-loss medications. The hormone GIP, on the other hand, usually promotes fat storage and can make it harder for people to lose weight.
AMG 133 combines these effects in a clever way. It includes both a GLP-1 agonist (a compound that mimics GLP-1’s effects) and a GIP antagonist (a compound that blocks GIP’s fat-storing effects).
This two-in-one approach has shown promise in early testing. The theory is simple: boost the body’s ability to feel full and burn calories while blocking the urge to store extra fat.
Promising Results from Early Studies
Researchers first tested AMG 133 in animals, where it reduced body weight significantly in both obese mice and monkeys. Encouraged by these findings, the team moved on to a small human trial. This early trial involved a group of adults with obesity, and participants received various doses of AMG 133 over a few months.
The results were striking. Not only did participants lose weight, but they continued to lose it long after the injections had stopped. In some cases, weight loss effects lasted up to 150 days following the final dose.
Besides helping with weight, AMG 133 also improved other key health markers, such as blood sugar levels and cholesterol.
These findings suggest that AMG 133 could have a long-term impact on metabolic health, potentially reducing the risk of diseases like diabetes and heart disease for those struggling with obesity.
Safety and Side Effects
Like any new treatment, AMG 133 has some side effects, mostly related to the digestive system. Some participants reported mild nausea and vomiting after their first dose, but these symptoms generally went away within a few days.
Importantly, there were no serious safety concerns reported in this early phase of testing. Researchers believe that further refining the treatment schedule and possibly introducing the dose gradually could help reduce these minor side effects even more.
What’s Next for AMG 133?
While AMG 133’s initial trial results are encouraging, it’s still early days for this potential treatment. The next steps will involve larger clinical trials to better understand its safety and effectiveness.
Researchers are also exploring how to optimize dosing, with the hope that the drug could be administered just once every few months. If successful, AMG 133 could be a game-changer, offering a new approach to weight loss that’s more effective, longer-lasting, and easier to manage than many existing treatments.
This breakthrough could be especially valuable for people whose obesity is resistant to standard diets and exercise routines.
A more effective, low-frequency treatment could relieve them of the daily or weekly routines required by most current weight-loss medications. AMG 133’s ability to target multiple pathways in the body could mean a major leap forward in addressing one of today’s most challenging health conditions.
Share this news
Related Science Stories
Recent Career Opportunities
-

Could a Simple Blood Test Spot Alzheimer’s...
Continue ReadingShare this news
What if a simple blood test could tell us who might develop Alzheimer’s disease years before symptoms appear?
This might sound like science fiction, but researchers have recently uncovered hidden clues in our blood that could bring us closer to this reality.
Alzheimer’s disease, a leading cause of dementia, gradually erodes memory and thinking abilities, affecting millions globally. The APOE-ε4 gene is a known risk factor, raising a person’s chances of developing Alzheimer’s by up to twelve times.
Yet, having the gene doesn’t guarantee Alzheimer’s, and many people with the disease don’t carry it. So, scientists are looking beyond genes, studying blood proteins to reveal new insights.
In a large study of over 5,000 older adults in Iceland, researchers used advanced technology to examine thousands of proteins in the blood. They found two types of protein “signatures” linked to Alzheimer’s.
One set of proteins changed in people who later developed the disease, regardless of whether they had the APOE-ε4 gene.
These proteins are involved in brain processes like neuron growth and communication, suggesting that early changes in the brain may be detectable in the blood long before symptoms emerge.
The second set of proteins, however, was deeply connected to the APOE-ε4 gene. For these 17 proteins, APOE-ε4 carriers experienced changes that were sometimes the opposite of those seen in people with Alzheimer’s.
For instance, in people with Alzheimer’s, some proteins essential for brain health increased, while these same proteins decreased in APOE-ε4 carriers, hinting at competing effects between the gene and the disease.
These findings are promising. They suggest that blood protein signatures might one day help us detect Alzheimer’s early and even reveal different disease pathways for those with or without the APOE-ε4 gene.
By understanding these distinct biological paths, scientists hope to tailor detection and treatment strategies to each individual’s unique genetic profile.
Though we’re still far from a simple blood test for Alzheimer’s, this study brings us closer.
It’s like finding pieces of a puzzle that could reveal the complex picture of Alzheimer’s and help guide us toward new preventive measures and treatments. One day, these protein clues could lead us to breakthroughs that transform how we detect and manage this devastating disease.
Share this news
Related Science Stories
Recent Career Opportunities
-

The Benefits of Dietary Protease: The Secret...
Continue ReadingShare this news
In a groundbreaking study led by Prof. Fang Chen’s research group at the National Engineering Research Center for Breeding Swine Industry, South China Agricultural University, a fascinating discovery was made.
This team explored whether adding a special ingredient to the diets of weaned piglets could improve their growth and health outcomes. The ingredient? Dietary protease, an enzyme that breaks down proteins, making them easier to digest.
The researchers conducted an experiment with 90 piglets, divided into three groups. Each group was fed a different diet over a 28-day period.
One group received a basic diet with composite enzymes but without protease (control group), another received a diet with no enzymes (negative control), and the last group received the same basic diet but with added protease.
The results were nothing short of remarkable. Piglets that received the protease-supplemented diet showed significantly improved growth performance. They gained more weight daily compared to their counterparts in the other groups.
But the benefits didn’t stop at just weight gain. These piglets also exhibited enhanced antioxidant capacity, indicating a better ability to combat oxidative stress—a vital factor for overall health and disease resistance.
The study delved deeper to understand how protease was making such a positive impact. One of the critical findings was related to the piglets’ gut health. Piglets on the protease diet had healthier intestines.
The protease helped in maintaining the integrity of the intestinal barrier, which is crucial for preventing harmful substances from entering the bloodstream.
Moreover, the protease-supplemented diet influenced the piglets’ immune responses. It reduced the levels of inflammatory markers and the expression of pro-inflammatory genes in the intestines.
This means the piglets were not only growing better but were also experiencing less intestinal inflammation, which can be a significant stressor and growth inhibitor.
Another exciting discovery was the positive shift in the intestinal microbiota—the community of bacteria living in the gut. The protease diet increased the abundance of beneficial bacteria while reducing harmful ones.
Beneficial bacteria like those from the Lachnospiraceae and Prevotellaceae families are known to aid in digestion and bolster immune health, creating a symbiotic environment where the piglets could thrive.
This study is more than just a win for piglets and their caretakers. It underscores the potential of dietary interventions in animal husbandry to promote better health and growth outcomes naturally.
By harnessing the power of enzymes like protease, farmers can improve the welfare of their livestock, reduce reliance on antibiotics, and support sustainable farming practices.
Share this news
Related Science Stories
Recent Career Opportunities
-

Is Your Child’s Bone Health at Risk?...
Continue ReadingShare this news
A group of researchers, led by Professor Emil Kääntä, decided to explore a troubling question: Does smoking during pregnancy make children’s bones more fragile?
The scientists gathered data from over 220,000 children born between 1987 and 1990. These children, now grown, have their health records carefully stored in Finnish medical databases.
The researchers wanted to see if there was a link between mothers who smoked during pregnancy and the number of bone fractures their children experienced as they grew up.
The results were startling. They found that children aged 5 to 15 years, whose mothers smoked while pregnant, had a higher risk of breaking bones. This was not a small increase – these children were 12% more likely to suffer fractures.
The scientists dug deeper and discovered that this risk was especially significant for non-high-energy fractures, like those that happen from everyday activities rather than serious accidents.
But why does this happen? The story unfolds with a look at how smoking affects a developing baby. When a mother smokes, harmful substances from the cigarettes can reduce the amount of calcium and nutrients the baby receives. This lack of nutrients can weaken the baby’s developing bones, making them more fragile as the child grows.
The researchers also noted that this increased risk of fractures was not due to other factors like the child’s activities or parental genetics. It was the smoking itself that was the culprit.
This discovery highlights an important message: Smoking during pregnancy can have long-lasting effects on a child’s health. Professor Kääntä and his team emphasize the need for preventive measures. They suggest that expectant mothers should receive better support to quit smoking to protect their children’s future health.
Share this news
Related Science Stories
Recent Career Opportunities



